Hypopneoa and sleep apnoea are not similar, but are related sleep disorders. A decrease in airflow is evident in hypopnea, lasting 10 seconds at the least in respiration. There is also a reduction in the saturation of oxygen and decrease in ventilation, thereby lessening the concentration of oxygen in one’s red blood cells. Hypopnoea can occur during nighttime while one sleeps, and during the day when one is awake.
Hypopnoea and Sleep Apnoea
Hypopnoea and sleep apnoea belong to the same family of sleep disorder. Where hypopnea is indicated by the partial obstruction of air during sleep or when awake, apnoea is indicated by the complete obstruction or blockage of air during sleep. Most often, these two occur simultaneously.
Doctors observed that patients with sleep apnoea sometimes experience only partial obstruction of air during sleep, instead of experiencing complete periodic obstruction. Sometimes, a combination of partial (hypopnea) and complete (apnoea) is manifested by patients. As a result of this discovery, sleep doctors concluded that a person may have hypopnea and sleep apnoea, and that a person diagnosed with hypopnea may eventually develop sleep apnoea.

What causes hypopnoea?
The causes of sleep apnoea and hypopnoea are very similar. Obstructive sleep hypopnea/apnoea is due to the relaxation of the muscles of the throat while one sleeps. Central sleep hypopnea/apnoea is due to the brain’s failure to signal the muscles to allow one to breathe.
As with sleep apnoea, there are risk factors for hypopnea. In the case of obstructive sleep hypopnea risk factors include: gender (more common in men), age, genetics, obesity, size of one’s neck, alcohol consumption, smoking, congested nasal passages, taking of sleep medication or sedatives. Other factors that could increase the risk of developing hypopnea include: heart disease, history of stroke, hypothyroidism, enlarges tonsils or adenoids in children, and other narcotics.
Are there treatment options?
As with sleep apnoea, there are treatment options for sleep hypopnea, and they depend on the severity and cause of the ailment. As with the causes of hypopnea, treatment options are the same as those of sleep apnoea.
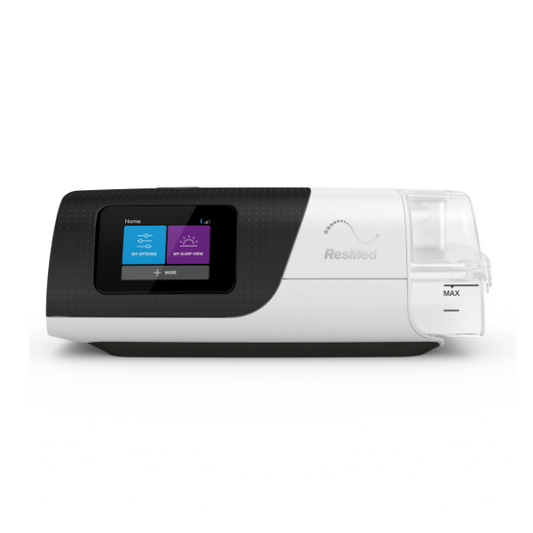
- CPAP or continuous positive airway pressure therapy
- Surgical removal of the obstruction if possible and applicable
- Usage of mechanical device to widen and stabilize the airway
Where hypopnoea is mild, changes on one’s lifestyle may actually decrease and eventually eliminate the condition. Lifestyle changes may include: eating a healthy diet, losing weight, smoking cessation, decreasing or completely stopping alcohol consumption, changing sleep positions, and avoidance of sedatives and other narcotics.
OSAHS or obstructive sleep apnoea-hypopnoea syndrome is a graver form of sleep hypopnoea or sleep apnoea. This condition is chronic and requires continuous management, and lifelong treatment.
Is hypopnoea preventable?
In cases of mild hypopnoea, symptoms can be eliminated by minor medical treatments and lifestyle changes. In the case of severe and chronic hypopnoea, management and treatment may take more time, and in some cases, a lifetime. However, all hope is not lost! As soon as symptoms manifest, it is best to consult with a credible physician. Early diagnosis and management will help reduce the severity of hypopoea, and the length of treatment.
Hypopnoea may not be preventable in some cases but taking steps to reduce the risks for developing hypopnoea is highly recommended.
Call us now for consultation and more information.