Scientific researches have indicated that the connection between Type 2 diabetes and obstructive sleep apnoea (OSA) is factual. Further studies suggested that the severity of a person’s sleep apnoea highly impacts his risk of developing type 2 diabetes.
Obstructive sleep apnoea is characterized by intermittent breathing during sleep. It is a sleep disorder that is linked to variety of problems not only in people with diabetes but to non-diabetics as well. OSA is associated to poor work performance brought about by disturbed sleep. OSA comorbidities include hypertension, arrythmias, stroke and even heart failure. A diabetic person with sleep apnoea may even develop insensitivity to insulin. With millions of people across the globe suffering from sleep disorder and diabetes, the risk for cardiovascular death has greatly increased.
Interaction between Sleep Apnoea and Diabetes
There are several mechanisms that link sleep apnoea and diabetes.
Inflammatory Reaction. Systemic inflammation, inflammation of the upper airways and inflammation of the lining of the blood vessels are associated with sleep apnoea. Obesity, high levels of triglycerides and cholesterol in the blood, cardiovascular disease and atherosclerosis are also linked to systemic inflammation.
Stress Reaction. The body is triggered to a fight or flight mode if it repeatedly deprived of oxygen due to sleep interruption caused by sleep apnoea. The stressor increases blood pressure and heart rate which could lead to cardiovascular disease, insulin resistance and chronic high blood pressure.
Lack of Oxygen. Repeated oxygen deprivation may prod the body to produce proteins associated with insulin resistance and glucose intolerance.
Cortisol Levels. Consistent sleep interruption may increase the cortisol level, leading to raised insulin secretion and blood glucose levels.
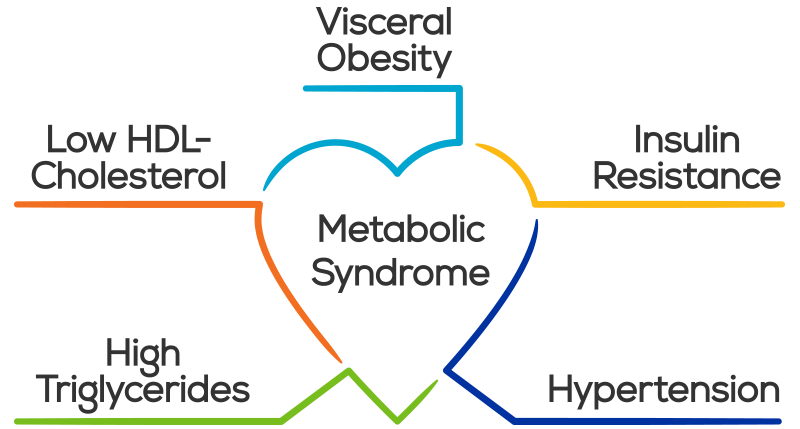
Link to Syndrome X
Syndrome X or metabolic syndrome is linked to sleep apnoea and type 2 diabetes. The syndrome is associated to five medical conditions that increases the risk of diabetes and atherosclerosis. The five medical conditions are high blood fasting glucose level, high blood pressure, abdominal fat, low HDL or food cholesterol, and high triglycerides.
Raised fasting glucose. Obstructive sleep apnea is linked with insulin resistance and glucose intolerance regardless if a person is obese or not. The condition has also been linked to insufficient sleep, interrupted sleep, and difficulty in sleeping and maintain sleep – all of which are associated with sleep apnoea and snoring
High Fat. Studies indicate that excess body fat in the abdominal area is a good indicator of sleep apnoea. Research shows that about two-thirds of people who snore or have sleep apnoea are obese. As the body-mass index (BMI) increases, the severity of OSA increases.
High blood pressure. The risk of high blood pressure also increases with increasing severity of sleep apnea, and it has additionally been linked with insulin resistance.
Low HDL and Triglycerides. People with type 2 diabetes commonly have reduced level of HDL or good cholesterol and elevated level of triglycerides, independent of BMI but relating to even a mild form of sleep apnoea.
OSA is independently linked to each of the five syndrome x conditions. In relation, the syndromes could be aggravated by untreated diabetes and sleep apnoea.
Treatment
Diabetic, OSA patients treated with CPAP therapy improved in management of their diabetes. This is an indication that sleep apnoea does have a part in the changes brought about by diabetes. A 1994 study of a group of men and women with OSA and type 2 diabetes received CPAP treatment for four months. After the prescribed length of therapy, the group’s sensitivity to insulin significantly improved.
A 2004 study gauged the effects of CPAP therapy on insulin sensitivity in a group of diabetic people with sleep apnoea. After three months of therapy, their sensitivity to insulin improved.
A 2005 study of 25 people with sleep apnoea and diabetes received a 4-hour CPAP therapy for four months. The study indicated that the group had improved blood sugar levels after meals, with lower HbA1c or glycosylated hemoglobin.
These studies reinforce the supposition that CPAP therapy is an efficient and effective component in the treatment of which the end goal is to improve the control of a patient’s blood sugar level, and to normalize his sleeping pattern.
Call us now for more information on OSA and CPAP therapy.