Obstructive sleep apnoea (OSA) and obesity hypoventilation syndrome (OHS) are related breathing disorders . OSA is characterized by interrupted sleep due to obstruction in the airway of persons who are most likely obese and with a body mass index (BMI) of over 30. Whereas patients with OHS are mostly obese and have sleep disordered breathing such as obstructive sleep apnoea.
What is Obesity Hypoventilation Syndrome (OHS)?
Obesity hypoventilation syndrome is a form of breathing disorder in people who are obese. The condition leads to high carbon dioxide level and to low oxygen level in the blood. This condition occurs due to hypoventilation during the day, which basically means that not enough air is moving in and out of the lungs persons suffering from OHS. In a nutshell, OHS is characterized by obesity, daytime hypoventilation and obstructive sleep apnoea. OHS is also known as Pickwickian syndrome as people with OHS manifest the symptoms described by Charles Dickens in his work The Posthumous Papers of the Pickwick Club.
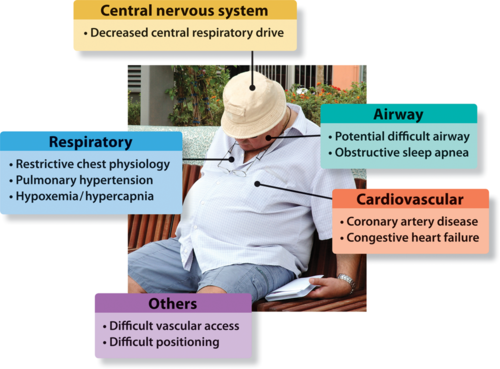
The cause (or causes) of obesity hypoventilation syndrome are not fully understood. It has been considered that the disorder is caused by the inability of the brain to manage a person’s breathing, or excess fat producing hormones that causes a person to breathe ineffectively, or the extra weight on the chest making it difficult to breather easily and normally.
Symptoms of Obesity Hypoventilation Syndrome
The primary symptoms of OHS are caused by low oxygen level in the blood and lack of sleep. Symptoms include lack of energy, daytime sleepiness, breathlessness and even depression. During sleep, a person with OHS will most exhibit loud and frequent snoring as well as pauses in breathing such as those exhibited by patients with obstructive sleep apnoea. The patient is unlikely to observe these nighttime symptoms, that those who sleep alone take a long time to realize that they have a breathing disorder.
Once diagnosed, OHS is treatable. If left untreated, the condition can be life-threatening as lack of oxygen strains the heart. The treatment will eliminate symptoms such as daytime sleepiness, fatigue, breathlessness, and reduce or entirely relieve depression. A patient’s quality of life will be vastly improved, with the probability of developing comorbidities greatly reduced.
Diagnosing Obesity Hypoventilation Syndrome
Early diagnosis of OHS means early treatment and reversal of symptoms. A doctor or health care provider will have to take a complete history of a patient, including his symptoms, evaluation of his BMI, sleeping habits and measurement of carbon dioxide and oxygen levels. The carbon dioxide and oxygen levels are measured by taking blood sample from an artery in the wrist. Another option is to use a pulse oximeter to measure the oxygen level in the blood. However, this process is not as accurate as blood sample from an artery. The doctor will most likely take a chest x-ray of the patient to rule out other possible causes of breathing difficulty. In case of severe sleep apnoea a polysomnography may be called for. This sleep study will help determine if the patient is suffering from obstructive sleep apnoea and help plan a course of treatment after a titration polysomnography is done.
Treatment for Obesity Hypoventilation Syndrome
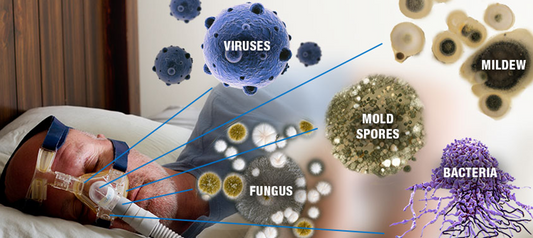
As with obstructive sleep apnoea, weight loss is the first approach in the treatment of OHS is weight loss. A combination of good diet and exercise, and a good night’s sleep are contributing factors to weight loss. For OHS patients with OSA, a proven effective treatment of obstructive sleep apnoea is positive airway pressure (PAP) therapy, which includes continuous PAP (CPAP) and Bi-level (BPAP) therapies. Once OSA is controlled, OHS treatment is well underway, as there are no medications for OHS yet.
If you think you or anyone you care about has undiagnosed OSA and OHS, give us a call. We can help!
1300 750 006